Newer than transvenous ICDs, subcutaneous ICDs work in a similar way. These devices are implanted under your skin near your armpit. An electrode is placed in the tissue to the left of your breastbone, not directly in your heart. Their leads do not go through veins.
How It Works
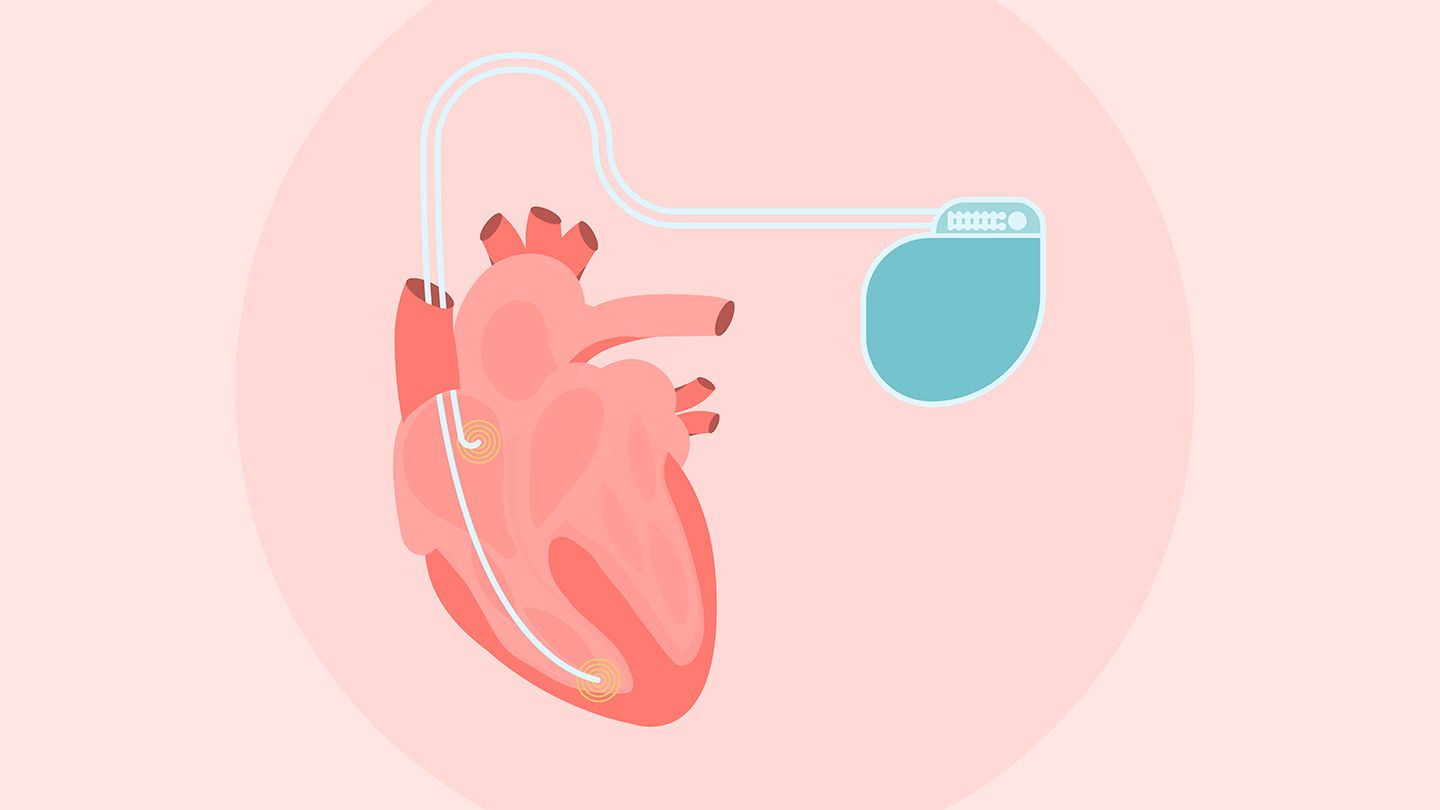
Subcutaneous ICDs have a pulse generator and an electrode sensor. Although the sensor isn’t actually inside your heart, it’s close enough to sense abnormal electrical activity and deliver shocks when needed. Subcutaneous ICDs can pick up heartbeats that are too fast but not ones that are too slow. Unlike transvenous ICDs, they can’t be used as pacemakers.
Subcutaneous ICDs are often as effective as transvenous ICDs in preventing sudden cardiac death in people with HCM. They may malfunction less often than transvenous ICDs, and they have the same likelihood of inappropriate shocks.
Implanting a subcutaneous ICD also is slightly less invasive than a transvenous ICD, because leads aren’t placed in your heart. But the procedure still involves general anesthesia or twilight sedation and, in some cases, an overnight stay in the hospital.
Who Is a Subcutaneous ICD For?
Subcutaneous ICDs are considered a suitable option for most people with HCM, especially those for whom the leads in a transvenous ICD pose a risk.
They’re not for people who may get too-slow heartbeats and need a pacemaker. They’re also slightly bigger than transvenous ICDs (about the size of a box of raisins), so they may not fit smaller bodies.
The battery life of a subcutaneous ICD also is usually lower than that of a transvenous ICD.
“I tend to use it in younger patients, patients with [an] elevated risk of infection or lack of vascular access, or patients with no pacing needs,” Dr. Chen says.
Read the full article here